Introduction: Vitamin D involves in several important human physiologic pathways from bone metabolism to inflammation and immune regulation. Patients who undergo hematopoietic stem cell transplant (HSCT) are at risk of developing vitamin D deficiency from various mechanisms and replacement of vitamin D in these patients can be challenging according to several reasons. In addition, vitamin D may potentially affect outcomes, overall health and quality of life after HSCT. An ultra-high dose vitamin D replacement was previously explored in pediatric HSCT patients but has never been investigated in adult patient population. In this study, we explored the incidence of vitamin D deficiency, the safety and efficacy of a single ultra-high dose vitamin D replacement including its effect on bone health among adult patients with hematologic malignancy undergoing HSCT.
Patients and Methods: First, we looked at the retrospective cohort of patients who underwent HSCT between January 2017 and August 2022 to explore the incidence of vitamin D deficiency (25-hydroxy vitamin D level <20 ng/mL) in Thailand. Subsequently, we prospectively included adult patients with hematologic malignancy undergoing both autologous (ASCT) and allogeneic HSCT (alloHSCT) from September 2022 to June 2023. All patients received a single ultra-high dose vitamin D on the day of admission prior to the initiation of conditioning regimens. We reported the safety and efficacy of a single ultra-high dose vitamin D (Ergocalciferol; Vitamin D2) replacement as calculated by weight and pre-transplantation vitamin D level among these patients using the Stoss protocol previously described. The effect of an ultra-high dose vitamin D on bone turnover was also monitored.
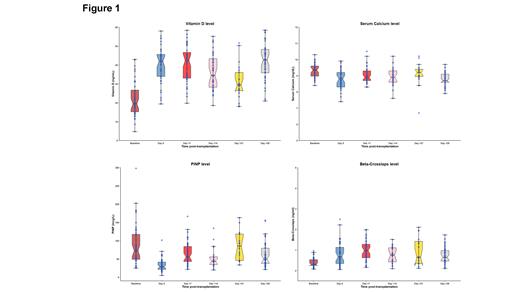
Results: In the retrospective cohort, 229 patients underwent HSCT (146 ASCT and 83 alloHSCT). Vitamin D deficiency was observed in 147 patients (64.6%) including 91 (62.3%) ASCT and 56 (67.5%) alloHSCT. The median 25-hydroxy (25-OH) vitamin D level was 17.6 (4.0-86.3) ng/mL comparable between autologous and allogeneic patients. In the prospective cohort, 45 patients underwent HSCT (27 ASCT and 18 alloHSCT). The median age of patients at the time of HSCT was 49 (23-67) years with 18 patients (40%) being male. The median pre-transplant 25-OH vitamin D level was 20.2 ng/mL with 22 patients (48.9%) (13 ASCT, 9 alloHSCT) meeting the criteria of vitamin D deficiency. The median dose of vitamin D2 used was 500,000 (300,000-600,000) IU. At day +28 post-HSCT, 40% of patients were able to attain 25-OH vitamin D level above 30 ng/mL comparable between ASCT and alloHSCT but significantly higher compared to the retrospective cohort. The time to neutrophil and platelet engraftment were 13 (9-26) days and 14 (9-33) days, comparable between the controlled retrospective cohort and high dose replacement prospective cohort. The median levels of parathyroid hormone (PTH) and bone turnover markers including osteocalcin, β-CrossLaps (β-CTx), and procollagen type I N-propeptide (PINP) at day+28 was 45.4 (19.4-152.2) pg/mL, 11.3 (6.0-16.8) ng/mL, 0.79 (0.1-13.0) ng/ml and 43.7 (19.7-133.7) mcg/L, respectively. Among patients who underwent alloHSCT, the incidence of cytomegalovirus reactivation and acute graft versus host disease was 72.2% and 11.1% (no grade 3-4), respectively. Figure 1 shows the kinetic of serum 25-OH vitamin D, Calcium, β-CTx and PINP of patients in the prospective cohort from baseline to day +28 post-HSCT. At all timepoints (day 0, +7, +14, +21, +28), the median level of vitamin D level was significantly higher whereas the median serum PINP level was significantly lower compared to the baseline level. There was no occurrence of hypercalcemia or bony events during the time of the study.
Conclusion: Our study highlights a high incidence of vitamin D deficiency in HSCT patients. Utilizing a single ultra-high dose vitamin D is an effective and safe approach to replace vitamin D in adult patients undergoing HSCT. A high percentage of patients could maintain adequate vitamin D level during post-transplant period. PINP level was sustainably decreased after vitamin D replacement indicating a lower bone resorption. Whether this approach will translate into improved immune function, long-term bone health and outcomes compared to the conventional replacement strategy warrants further exploration in prospective randomized clinical trials.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal